(The original language of this article is French, and the graphs are shown from actual screenshots)
Malnutrition is a condition characterized by a loss of body mass greater than 5% in 1 month according to the Haute Autorité de Santé (French National Authority for Health)¹, which can develop during aging. Its causes are generally a decrease in food intake combined with an increase in protein breakdown². Moderate malnutrition can lead to a state of frailty in the elderly, meaning a vulnerability to events that could quickly degrade their quality of life or even their health status (illness, risk of falls, etc.). When malnutrition is severe, it can even lead to death, making it crucial to prevent and detect it early enough to manage it as effectively as possible. In this context, bioimpedance analysis is an effective and relevant tool due to its ability to quickly assess body composition, leading the Haute Autorité de Santé to recommend its use for malnutrition screening¹. It is also useful in the monitoring and evaluation of the body composition of a malnourished person to quantify the effects of nutritional management.
In this case study, the body composition of an elderly person with malnutrition will be presented to understand the consequences of malnutrition on body composition and thus facilitate its detection and management.
| Gender | Female |
| Age | 80 years |
| Height | 159 cm |
| Weight | 44,1 kg |
| BMI | 17,44 kg/m² |
| Pathologies | Malnutrition |
Quick Analysis

Firstly, we can observe that this person has a body fat mass (-6.10 kg) and skeletal muscle mass (-2.97 kg) significantly below the health references for her age, demonstrating the presence of severe malnutrition. Surprisingly, the hydration level of this patient is very high (+2.46 L), which is a consequence of her malnutrition and whose potential causes will be explained later in this case study. The bone mass index also indicates a significant bone deficit (-19%), characteristic of osteopenia in this patient.

The phase angle value for this patient is below the lower limit for her age, indicating a highly degraded health status, which is confirmed by the impedance ratio (IR) value far exceeding the threshold for women, which is 0.82. These two values confirm that malnutrition causes a significant deterioration in the health status of this patient, and over time, it will be relevant to 1) monitor the evolution of the physiological state of this patient and 2) control the effects of nutritional management on it.
Fat Free Mass, Appendicular Skeletal Muscle Mass, and Fat-Free Dry Mass
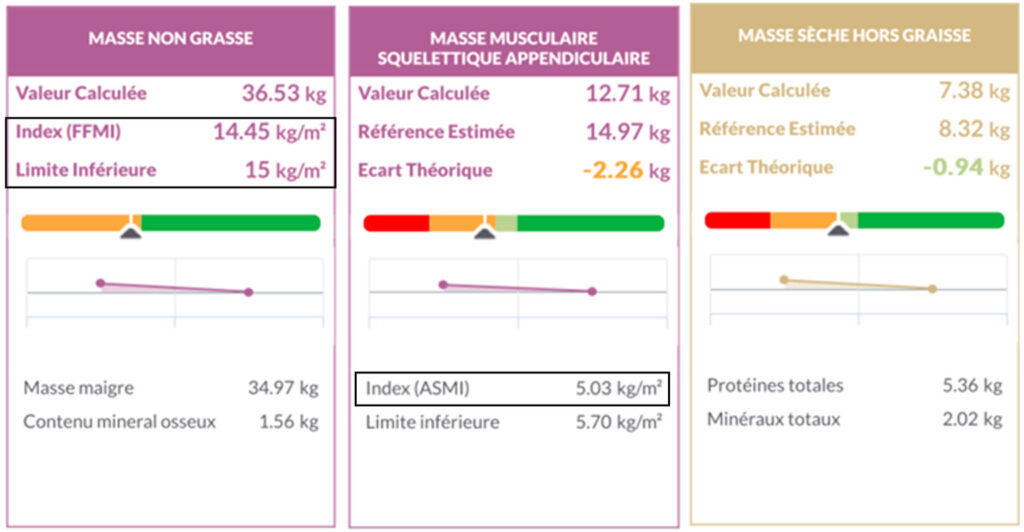
The main diagnostic marker of malnutrition recommended by the HAS (French National Authority for Health) is the fat-free mass index (FFMI) with a threshold of 15 kg/m² for women and 17 kg/m² for men. In the case of this patient, her FFMI is 14.45 kg/m², confirming that she is malnourished according to these criteria. From a body composition modeling perspective, fat-free mass corresponds to all the components of the human body except for the lipids in adipose tissue, including proteins, minerals, and water. Among the organs constituting fat-free mass, skeletal muscles are the majority, accounting for 48 to 55% depending on the individual. As they are responsible for locomotion and the ability to perform daily tasks, it is important to monitor muscle mass in the context of malnutrition. Here, we can observe that the appendicular skeletal muscle mass, i.e., of the limbs, is 2.26 kg below the health reference with an appendicular skeletal muscle mass index (ASMI) of 5.03 kg/m², confirming the presence of sarcopenia in this patient. These results show that severe malnutrition causes a significant decrease in the patient’s skeletal muscle mass and, therefore, her ability to perform daily tasks, even the simplest ones.
Fat-free mass and skeletal muscle mass are two compartments with high hydration rates (73.2% and 75%, respectively), so a reduction in these two masses could be caused by dehydration, a common event in the elderly. It is therefore necessary to check if these deficits are caused by a decrease in overall protein mass, which can be verified by fat-free dry mass. In the case of this patient, the overhydration observed in the quick analysis strongly suggests a protein mass deficit, which is confirmed by the fat-free dry mass value being 0.94 kg below the health reference.
Hydration

As mentioned in the quick analysis, the patient presents a high overhydration both in total body water (+2.37 L) and fat-free hydration (+2.46 L), which corresponds to the total water volume without the water in adipose tissue. This result may seem surprising considering the high prevalence of dehydration in this population, but the presence of systemic edema is common in malnutrition, particularly if it is severe³. This edema could have two origins:
- Degradation of the extracellular matrix, particularly in the blood vessels, associated with a decreased drainage capacity of the lymphatic system, leading to water accumulation in the interstitial tissues⁴.
- Muscle damage and localized inflammation caused by malnutrition, which are responsible for intramuscular edema as seen in myopathies⁵.
Consequently, the accumulation of water can be either extracellular (accumulation in the interstitial tissues) or intracellular (intramuscular edema), which can be determined through the “Water Balance” and “Fat-Free Water Balance” tiles.

In the case of this patient, we can observe significant intracellular overhydration on these two tiles, suggesting the presence of intramuscular edema and little water accumulation in the interstitial spaces. However, even though the majority of the excess water is intracellular, there is also a surplus of 450 mL extracellularly, indicating a more modest water accumulation in the extracellular space.
Fat Mass with Constant Hydration and Bone Mineral Content

Malnutrition is generally characterized by a decrease in daily food intake that the body compensates for in two ways:
- By breaking down intramuscular proteins to provide the amino acids necessary for the synthesis of proteins that ensure the functioning of other organs.
- By breaking down lipids from adipose tissue to provide the energy necessary for the body’s functioning.
Consequently, it is important to monitor the percentage of fat mass to determine if the body is capable of compensating for the energy deficit, particularly while nutritional management allows for a return to normal physiological functioning. In the case of this patient, she has a fat mass percentage of 18.18%, which is a deficit of 6.10 kg compared to the health reference, indicating that she has a reduced but still sufficient fat mass to compensate for the energy deficit.
Conversely, the patient has a deficit of 360g of bone mineral content, indicating the presence of osteopenia and thus an increased risk of fracture in case of a fall. Considering her low muscle mass, it is highly likely that she has difficulty moving or standing, which also increases the risk of falls. During nutritional management, it is therefore also necessary to provide sufficient minerals and nutrients to promote a return to a normal bone mass value.
Conclusion
Malnutrition is a pathological condition characterized by a loss of protein mass leading to a decrease in fat-free mass and skeletal muscle mass, as seen in this patient. These two parameters are the most useful and relevant for detecting and managing malnutrition, however, it is also necessary to check hydration if edema is present, as well as fat mass and bone mineral content, in order to adjust the management plan.
References
- Haute Autorité de Santé [Internet]. [cité 21 déc 2022]. Diagnostic de la dénutrition de l’enfant et de l’adulte. Disponible sur: https://www.has-sante.fr/jcms/p_3118872/fr/diagnostic-de-la-denutrition-de-l-enfant-et-de-l-adulte
- Cruz-Jentoft AJ, Kiesswetter E, Drey M, Sieber CC. Nutrition, frailty, and sarcopenia. Aging Clin Exp Res. févr 2017;29(1):43‑8.
- White JV, Guenter P, Jensen G, Malone A, Schofield M, Academy Malnutrition Work Group, et al. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr. mai 2012;36(3):275‑83.
- Gonzales GB, Njunge JM, Gichuki BM, Wen B, Ngari M, Potani I, et al. The role of albumin and the extracellular matrix on the pathophysiology of oedema formation in severe malnutrition. EBioMedicine. 7 avr 2022;79:103991. 5.
- Poliachik SL, Friedman SD, Carter GT, Parnell SE, Shaw DW. Skeletal muscle edema in muscular dystrophy: clinical and diagnostic implications. Phys Med Rehabil Clin N Am. févr 2012;23(1):107‑22, xi.