(The original language of this article is French, and the graphs are shown from actual screenshots in the original language)
The ketogenic diet is characterized by a high lipid intake (70-80% of intake) combined with a reduced carbohydrate intake (5-10%) and a normal protein intake (15-20%)¹. Although known and used for a long time in the treatment of epilepsy², it has seen a resurgence of interest in the management of obesity, both for its ability to rapidly reduce fat mass (FM) and for its metabolic and cardiovascular benefits. Indeed, in a recent meta-analysis, Choi et al.³ showed that the ketogenic diet improved glycemic control and lipid profile in obese patients, with or without type II diabetes. These benefits are explained by two main mechanisms¹:
- The significant reduction in carbohydrate intake causes a decrease in insulinemia, thus increasing the insulin sensitivity of cells.
- The significant increase in ketogenesis and a reactivation of lipolysis, which allow for a greater consumption of triglycerides from adipose tissue to produce 1) energy from fatty acids and 2) ketone bodies that replace glucose in several organs.
Despite significant beneficial effects, several limitations seem to be present in this diet, including a possible lipid overload at the plasma level and difficulty maintaining this diet over time². Moreover, it also seems that the quality of lipids is important in the effects of this ketogenic diet. However, these data suggest that using this diet could be interesting occasionally to induce fat mass loss and metabolic improvement before establishing long-term healthy dietary habits.
Another approach that has seen a resurgence of interest is fasting, which can be practiced in various forms, ranging from intermittent fasting, where food intake is limited to 4-8 hours a day, to dry or water fasting. From a physiological point of view, fasting has numerous metabolic benefits as well as benefits for the quality of human body cells through its ability to activate autophagy, a biological phenomenon involved in cellular renewal⁴. Among the beneficial effects of fasting at the metabolic level, we can observe an increase in insulin sensitivity, a decrease in insulin production by the pancreas, and an increase in lipolysis⁵. Therefore, fasting has similar effects to the ketogenic diet, and both seem to be complementary approaches in the nutritional management of obese individuals.
In this case study, we propose to study the nutritional management of an obese patient combining a ketogenic diet, fasting, and lifestyle modifications.
| Sex | Male |
| Age | 48 years |
| Height | 177 cm |
| Weight | 126,7 kg |
| BMI | 40,4 kg/m2 |
| Waist Circumference | 102 cm |
| Pathologies | Obesity |
Patient Characteristics
At the blood level, this patient had a good cholesterol profile; however, the CRP concentration was 1.55 mg/L and ferritin was 338 µg/L, indicating low-grade inflammation and iron overload, respectively. This patient also had hypertension which is being managed with medication.
In addition, he had a lifestyle that favored his condition, characterized by significant sedentary behavior, an unbalanced diet, poor hydration, associated with a high daily consumption of sodas and poor-quality sleep.
Quick Analysis


The quick analysis of the results shows that this person has an excess FM of 14.43 kg compared to his reference as well as a skeletal muscle mass (SMM) higher by 17.83 kg. The SMM and bone mass (BM) indices confirm that these two parameters are elevated in this patient and are sufficient to support the excess FM, which is confirmed by the muscle load and total load indices. These results also suggest that the SMM and BM are sufficient to facilitate the implementation of appropriate physical activity in the management. Surprisingly, it is interesting to note that this patient has hydration close to perfect hydration, which contrasts with the values obtained in individuals with a comparable BMI. Finally, this patient’s phase angle is high and could be interpreted as a sign of good cell quality; however, it should be noted that the phase angle is closely related to the total number of cells in the body, which is very high in obese patients. Thus, high phase angles have already been shown in obese individuals⁶, making it difficult to use this parameter for a punctual evaluation of cell quality in these patients. It remains interesting to use in monitoring the general condition of patients and to observe any possible deterioration in their clinical condition.
Fat Mass at Constant Hydration, Total Skeletal Muscle Mass, and Limb Skeletal Muscle Mass
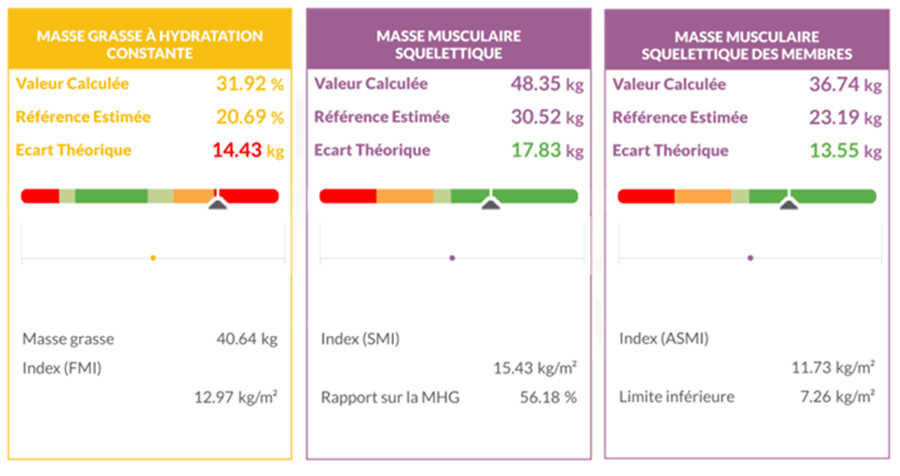
The analysis of the various tiles of fat mass (FM) at constant hydration, skeletal muscle mass (SMM), and appendicular skeletal muscle mass (ASMM) confirms the observations of the quick analysis. Indeed, the patient has an FM of 40.64 kg, resulting in a body fat percentage of 32%, and an SMM of 48.35 kg, resulting in a fat-free mass (FFM) ratio of 56.18%.
This ratio confirms that SMM is a very important part of the FFM and is sufficient to ensure adequate physical activity. This result is also reinforced by the ASMM, which is very high and suggests significant skeletal muscle mass in the legs, thus facilitating the performance of physical exercise.
Patient Characteristics
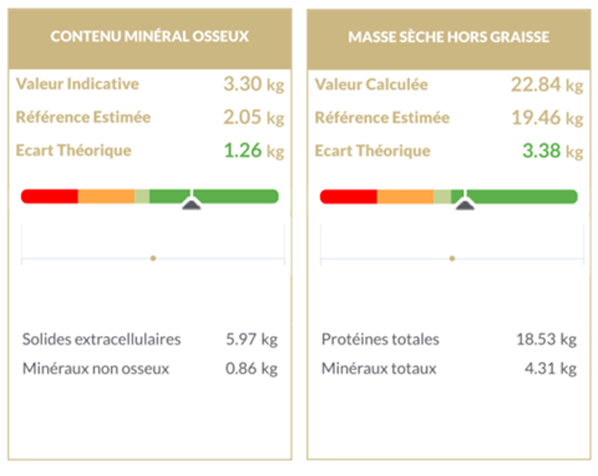
Bone mineral content (BMC) corresponds to the amount of minerals in the bones and is an indicator of bone mass. In this patient, we can observe a very high BMC compared to his reference, indicating that he has sufficient bone mass to support all the SMM and FM. Moreover, this parameter also suggests that bone mass will be sufficient to support the increased mechanical stresses related to exercise, so he may be able to support higher intensity exercises than walking or swimming, such as resistance exercises like crosstraining/crossfit and weight training.
Fat-free dry mass is a parameter that corresponds to the total proteins and minerals contained in the body, thus constituting a complementary parameter to SMM, ASMM, and BMC. Although it is less relevant in a punctual evaluation, it is a very useful marker in monitoring the three previously mentioned parameters as it allows confirming that a change in SMM, ASMM, or BMC is related to a change in protein and/or mineral content. Here, the high value of fat-free dry mass is consistent with the observed SMM and BMC.
Hydration
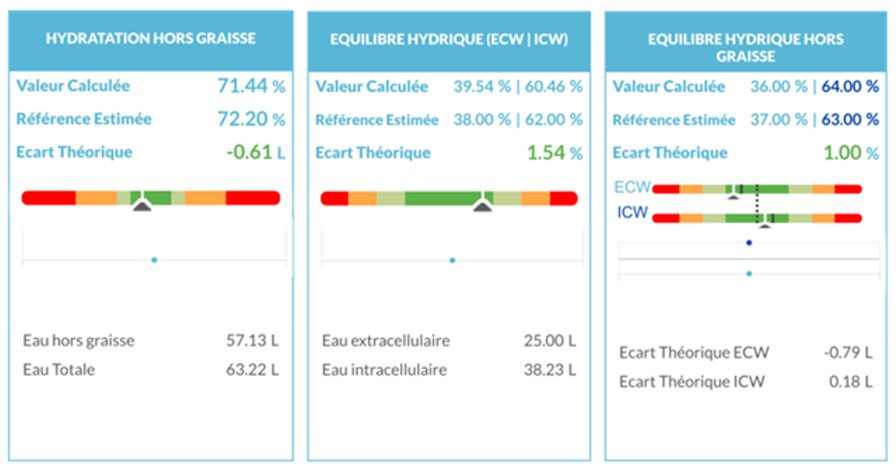
This patient also presents almost perfect hydration, contrasting with the results generally obtained in obese individuals, who present chronic dehydration⁷. We can also observe that total and water balance are maintained despite slight intracellular overhydration. These results indicate that despite altered water intake and hypertension, it seems that this patient’s tissue hydration is normal.
Description of the Management
From a nutritional standpoint, the proposed management included:
- A ketogenic diet during the first months of management, followed by a transition to a Mediterranean diet alternated with ketosis periods. Both diets were combined with intermittent fasting to create a caloric deficit and initiate weight loss.
- The goal of combining both is to maintain the physiological benefits of both approaches, allowing for metabolic flexibility while achieving a caloric deficit leading to weight loss.
- A return to physical activity starting with walking and then gym workouts (strength training/aerobic exercise).
- An improvement in hydration by replacing soda with water daily.
- An improvement in sleep quality, notably by going to bed earlier.
Management Results
After one year of management, the patient lost 32 kg of body mass and 26 cm of waist circumference. Blood results show that low-grade inflammation has disappeared, oxidized LDL is absent, and cholesterol profile is normal. Additionally, glycemic regulation improved with increased insulin sensitivity and decreased insulinemia, reflecting a significant reduction in insulin resistance. Finally, ferritinemia also decreased, though still higher than normal, suggesting an improvement in iron metabolism.
In terms of management, the Mediterranean diet combined with intermittent fasting and ketosis periods is maintained, along with the lifestyle habits acquired in physical activity and sleep.
Fat Mass at Constant Hydration
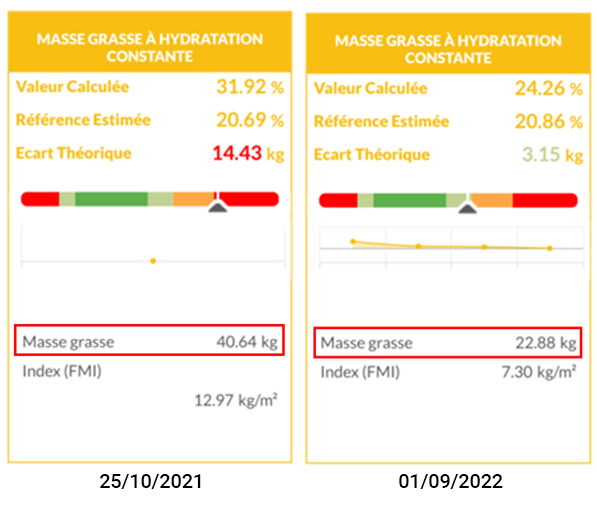
After one year of management, the patient lost 17.76 kg of fat mass, reducing from 31.92% to 24.26% fat mass.
Total Skeletal Muscle Mass, Appendicular Skeletal Muscle Mass
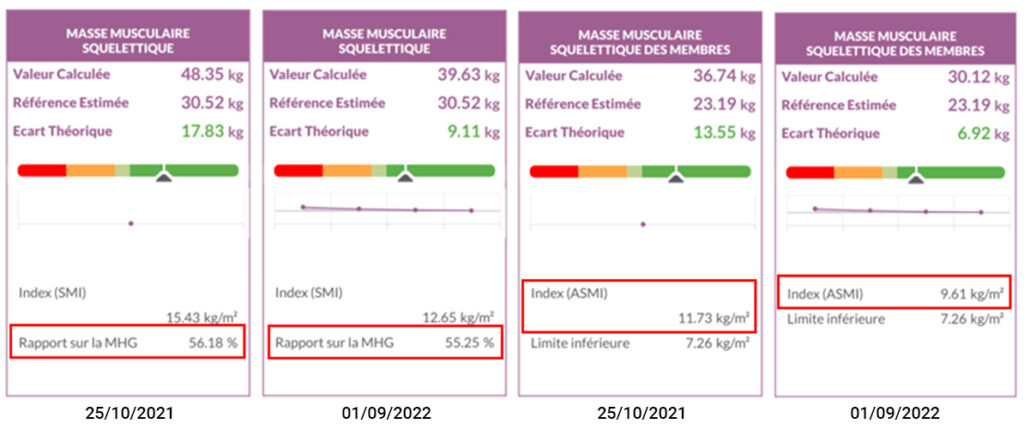
We can observe that during the year, the patient lost 8.72 kg of SMM and 6.62 kg of ASMM. Although these losses seem significant, they may result from water loss rather than a loss of contractile proteins, which can be verified by the fat-free dry mass. Despite this loss, if we consider the ratio of SMM to fat-free mass as well as the ASMI, it seems that the patient’s SMM is still sufficient to perform daily activities.
Fat-Free Dry Mass and Bone Mineral Content
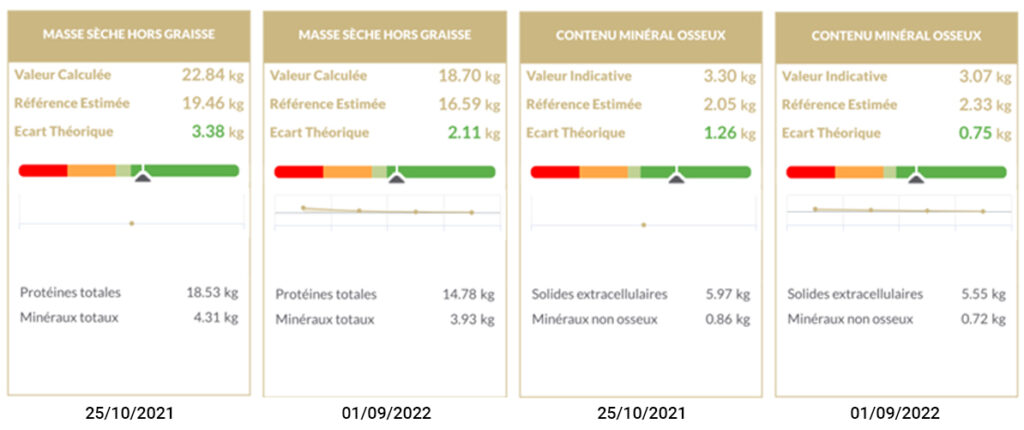
Between the two measurements, the loss of fat-free dry mass was 4.14 kg and that of BMC was 230 g. If we consider the loss of SMM along with the decrease in fat-free dry mass, it would appear that the management has reduced the contractile proteins of the SMM by about 4 kg.
This loss can have two origins: an insufficient protein intake in the diet and/or a return to a muscle mass suitable for the total body mass. Indeed, the increased muscle mass present in people with obesity is closely related to the excess total body mass. Functionally, skeletal muscle resists mechanical stresses by producing enough force to avoid excessive tension on the muscle fiber membrane. Therefore, an increase in stresses on the muscle membrane means that the force produced by the muscle is not sufficient. Physiologically, this activates muscle protein synthesis to increase its mass and thus its strength. In the context of obesity, this normal physiological mechanism is responsible for the high muscle mass in these subjects. The loss of SMM can thus be explained by the decrease in mechanical stresses applied to the skeletal muscle, slightly reducing protein synthesis and thus intramuscular protein mass.
The slight loss of BMC can also be explained by this decrease in mechanical stresses applied to the skeleton, reducing bone mineral synthesis and allowing a new normal value to be reached.
Hydration

Fat-free hydration is also maintained after weight loss, although a total water loss and fat-free water loss of 10.20 L and 7.57 L, respectively, can be observed. The total water loss between the two points is mainly explained by the decrease in the amount of lipids in the FM and proteins in the SMM, leading to water loss.
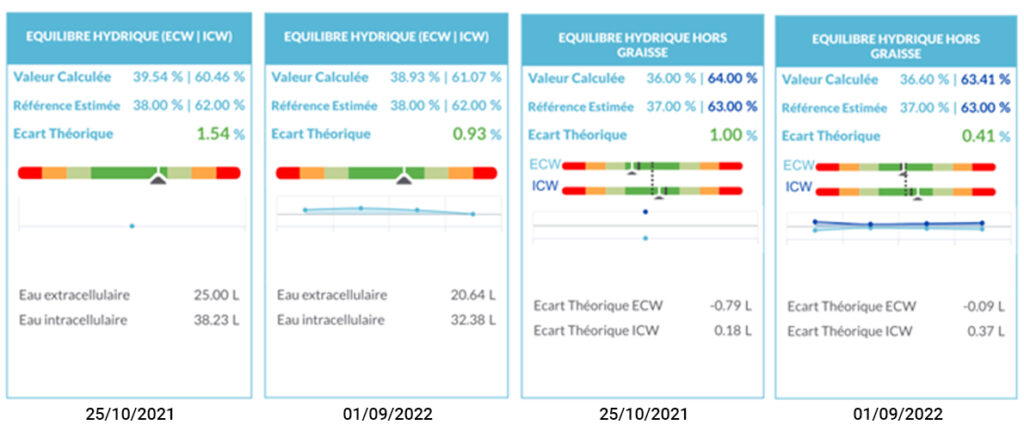
We can also observe that total and fat-free water balances are maintained following the management. If we consider these results alongside the nutritional modifications and the improvement in cardiovascular health, it seems that this management has created a protective physiological environment against the development of cardiovascular complications commonly present in obese patients⁸.

Phase Angle
Despite a slight decrease, the phase angle remains high following the management, decreasing from 7.7° to 7.2°. When correlating this change with the loss of body mass, the phase angle has remained relatively stable despite the significant loss of cellular mass. Thus, this result indicates that the management has improved cell quality, which is confirmed by the reduction in inflammation and insulin resistance.
Conclusion
In conclusion, the bioimpedance data obtained during the management of this patient show that a nutritional management combining ketogenic/mediterranean diet, intermittent fasting, appropriate physical activity, and better sleep quality allows for significant improvement in body composition in this obese patient. Additionally, the blood results also indicate significant benefits of this management on inflammation and insulin metabolism.